Hepatitis A,B,C,D
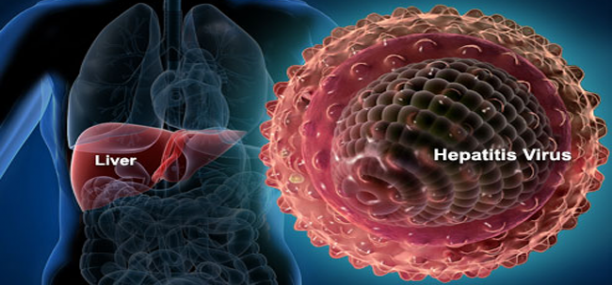
Hepatitis (вирусные гепатиты التهاب الكبد الفيروسي), an inflammatory infectious disease of the liver, it is caused by RNA containing viruses HAV, HBV. HCV, HDV
Pathogens – hepatitis viruses A,B,C,D
Epidemiology
Active Infection
In Hepatitis A the person is having an infection in pre jaundice period and in the 1st 3-7 days of jaundice (icterus, желтухи, الصفيرة ) in hepatitis B, D, C the patient is infected and/or a carrier of the virus in all periods.
Route of Contamination
In HAV infection, the virus spread by oral fecal route, by ingesting contaminated food, water, or by contact.
In HBV, HDV, HCV the virus spread by parenteral exposure, transmission through contaminated blood, or by sexual contact when infected blood or OPIM are introduced directly into blood or through a break in your skin.
HBV can pass by vertical transmission, from an infected mother to her fetus through the placenta in pregnancy or from the mother to her newly born child in labor, less commonly the virus can spread in saliva and/or in breast milk.
Clinical picture
Incubation period for HAV ranges between 2x weeks to 2x months, in HBV incubation period ranges between 2x to 6 months, in HCV incubation period ranges from 6-12 weeks
HDV usually coexists with other underlying infections, in most cases it presents as a co infection with HBV, or following HBV infection (super infection)
Prodromal preicteric period, it may show in one of the following variants:
- Flu like symptoms
- Dyspeptic – acute disease, lasting for a period of 4-6 days, which is a characteristic feature of HAV
- Astheno-vegetative, arthralgic, or both of them; however, the following symptoms are characteristic features of HBV.
Intoxication syndrome, weakness, anorexia, nausea, vomiting, adinamia, sleeping disorders (feeling sleepy in the day, insomnia or the inability to sleep at night), bradycardia, low grade fever, in severe conditions, encephalopathy may show.
Jaundice, icteric sclera and skin, darkened urine, acholic stools, pruritis of the skin
Hepatomegaly, usually accompanied by splinomegaly
Hemorrhagic syndrome, limited to severe conditions of hepatitis and is characterized by nasal, uterine, or gum bleeding, and hemorrhagic skin
In HCV infection jaundice is absent, while all the other symptoms are severe.
Chronic process develop in 50% of cases with HBV, and 80-85% in HCV, hepatic cirrhosis may develop in the terminal stage with hepatic carcinoma
Hepatic coma and heavy intoxication symptoms such as nausea and vomiting, symptoms of encephalopathy, tachycardia, hemorrhagic syndrome (bleeding in the internal organs), abdominal pain, the liver may decrease in size, the smell of the liver can be felt from the mouth may develop in severe cases of HBV infection.
Complications
- Acute and pre-acute dystrophy of the liver, hepatic encephalopathy
- Functional and infectious diseases of the bile ducts
Differential diagnosis
Differential diagnosis to be made with supra hepatic jaundice (commonly of hemolytic characters), liver cirrhosis, or with various bile duct tumors, gallbladder stones, as well as with other disorders causing jaundice such as arsenicosis, leptospirosis, infectious mononucleosis.
Lab Tests
Biochemical Tests
- Syndrome cholestasis, increased bilirubinum (direct), increased cholesterol, alkaline phosphatase, gamma glutamate transpeptidase.
- Cytolysis syndrome -increased levels of alanine and aspartic transaminase (ALT and AST).
- Mechanical inflammatory syndrome – decreased levels of albumin, increased levels of beta 2 and gamma globulins, increased thymol and decreased sublimate samples.
Serological Tests: Based on the detection of specific antigens of viruses and antibodies to them:
- In HAV, identified antibodies to the virus class M (anti-HAV IgM).
- In HBV, identified HBsAg (appears in the middle of the incubation period, and in general it is stored within a month from the beginning of jaundice), HBeAg (appears in the middle of the incubation period, and decrease significantly with the emergence of jaundice), antibodies to HBeAg (appear following the 1 – 2 weeks of jaundice) НВсоr IgM antibodies (throughout the acute phase) antibodies to НВсог IgG (appear in the subacute phase and is stored for many years).
- In HCV, identified antibodies to the antigen related to hepatitis C virus (anti-HCV IgM and IgG).
- In HDV, identified anti-HDV IgM and IgG that are usually present with HBV markers.
To assess the proper elimination of the pathogen from the body, polymerase chain reaction (PCR) has been widely used to rule out patients with serum HBV DNA and HCV RNA.
Treatment.
Causal treatment (Etiotropic therapy) of acute viral hepatitis does not apply; however, evidence of benefits in the prevention of progressive parenteral viral hepatitis by using interferon 2 “alpha” (Roferon A, Intron A, velferon…) do exist.
Pathogenetic therapy comprises administering the detoxification agents (gemodez, neogemodez, reomakrodeks, 5% glucose solution, etc.).
Recommended antioxidant drugs (Riboxinum, ascorbic acid), vitamin B, chelators.
When indicated – Antiplatelet agents (heparin). The advisability to use cholekinetic drugs must be addressed individually
In the period of convalescence (magnesium sulfate, Flamin, berberine, etc…).
Choleretic drugs (allochol, cholenzim…), Hepatic protectors (Essentiale, legalen…). In severe viral hepatitis corticosteroids, hemosorbtion, and plasmapheresis are recommended.
Verified by: Dr.Diab (January 7, 2017)
Citation: Dr.Diab. (January 7, 2017). Hepatitis. Medcoi Journal of Medicine, 4(2). urn:medcoi:article15841.












There are no comments yet
Or use one of these social networks