How to Diagnose Cushings syndrome
Cushings syndrome (hypercortisolism, or ectopic ACTH syndrome) is an adrenal disorder caused by a pituitary tumor and characterized by cortisol overproduction that arises in response to excessive ACTH secretion. ACTH regulates and stimulates the secretion of cortisol in the adrenal cortex.[1][2][3]
Pathogenesis of hypercortisol
A high blood cortisol level can be caused by:
(1)– Pituitary tumor, is the most common cause of cushing’s syndrome, it accounts for 60 percent of cases. This condition is termed cushing’s disease. Moreover, increased levels of serum cortisol and serum Acth are characteristic diagnostic findings of this condition.[29][30]
(2)– Adrenal tumor is a common cause of increased blood cortisol levels; Moreover, increased serum cortisol level and decreased ACTH are characteristic diagnostic findings of this condition, as increased serum cortisol reduces ACTH production in the pituitary. The two main types of adrenal tumors:
- Adrenal adenoma, found to be the reason in 25% of cases.[32]
- Adrenal carcinoma, in 10% of cases cancer of the adrenals can cause the disease, letrogenic steroids.[31]
(3)– The condition may be triggered by an overproduction of ACTH outside of the pituitary, which is independent of circulating cortisol levels just like in lung cancers (5% of cases).[33][34]
Diagnostic symptoms of Cushing’s syndrome
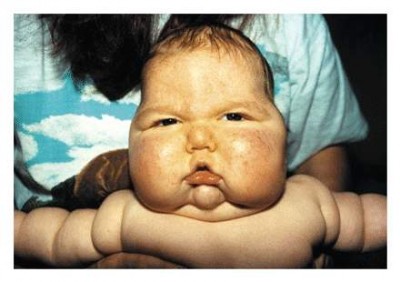
The following signs and symptoms increase your chances of having Cushing’s syndrome:
Central body obesity and weight gain, especially around the hips. Overactive adrenals produce excessive amounts of cortisol, which in turn increase blood glucose levels. The increased circulating concentration of glucose stimulates the pancreas to secrete insulin that acts on specific target cells in the muscles, liver and adipose tissue stimulating them to increase the glucose uptake and storing it as glycogen in the muscles, adipose tissue and liver where glucose is converted into triglycerides or fat.[1][4][5]
Hypertension is a major diagnostic criteria for the diagnosis of Cushing’s disease, it is characterized by a systolic blood pressure of ≥140 mmHg and diastolic blood pressure of ≥90 mmHg.[7]
Glucose intolerance is a prediabetic state of hyperglycemia associated with insulin resistance. The over secretion of cortisol increases the blood sugar level, and the amount of insulin secreted in response to a meal can no longer keep the blood sugar level within normal bounds. With time patients will start to suffer of symptoms related to excess glucose just like diabetic patients, a term medically known as Glucose intolerance, such symptoms include frequent urination, unjustified thirst, hunger, weight gain, and weakness.[26][27][28]
Excess hair growth or hirsutism refers to the untypical growth of dark thick hair in areas where females typically grow fine invisible hair. Consistently high plasma concentration of cortisol can threaten homeostasis (the internal cellular balance), by manipulating the estrogen-testosterone balance. Cortisol is a steroid synthesized of five cholesterol based enzymes; however, with chronically elevated ACTH levels, the normal adrenal cells will fail to respond normally by synthesizing the five enzymes, as chronic increased secretion often causes lack of one of the various enzymes, and the cells of the adrenal cortex will start releasing other hormone precursors to cortisol such as testosterone (an adrenal androgen), which is common in people with 21-hydroxylase deficiency.[8][9][10]
Osteoporosis is a condition characterized by loss of bone tissue and diminution of bone density without a defect in mineralization, as the amounts of phosphorus, calcium and vitamin D are commonly sufficient; however, it often results because the rate of bone resorption exceeds the rate of bone synthesis (formation), as the process of blasting or building bone cells (osteoblast) is related to estrogen and testosterone, so when estrogen or testosterone level drops osteoclast activity increases (the process of bone resorption).[11][12][13]
Kidney stones is a common symptom of Cushings syndrome, as chronic disease impairs the functionality of renal tubules. Moreover, chronically increased blood sugar levels result in urinary frequency and hypertension. Cystine is an amino acid poorly soluble in urine, especially in acidic and highly saturated urine, which is common in patients with frequent urination. Furthermore, a reduced urine volume often leads to impaired renal reabsorption of cystine in the impaired renal tubules, which increases the urinary cystine concentration, and when the urinary cystine concentration exceeds its solubility, crystals and stones are formed due to precipitation.[14][15][16]
Menstrual irregularity is a menstrual disorder caused by a variety of conditions. Common manifestations include menorrhagia (prolonged menses) or polymenorrhea (frequent menstruation), which is usually caused by a functional abnormality in the hypothalamic–pituitary–gonadal axis (HPG axis) that regulates homeostasis in the female body (the balance between hormones regulating menstruation); however, normally bleeding is stimulated by estrogen, but in Cushings syndrome menstrual irregularity is usually caused by pituitary dysfunction and endocrine disorder (excess androgens produced by the adrenals), which often results in Amenorrhea.[17][18][19]
Emotional lability (Pseudobulbar affect, PBA, or emotional incontinence) is a psychotic episode characterized by involuntary episodes of crying and/or laughing.[20][21][22]
Thinning of the skin and dryness, are manifestations of increased weight, which will stretch the skin and cause hemorrhage with red or purple striae on the trunk, buttocks, arms and breasts. Moreover, impaired wound healing and easy bruising may be attributed to defects in the normal tissue.[23][24][25]
Testing
The total 24-hr cortisol production is elevated in patients with Cushing’s syndrome, as they usually have an elevated cortisol level all day long; Moreover, the level of cortisol peaks early in the morning and keeps rising during the day, since in such patients the normal diurnal decline in cortisol production is absent; however, the night plasma cortisol levels are also elevated. Normally, the plasma cortisol levels range from about 5 to 25 micrograms per deciliter (ug/dl) in the early morning (6-8am) and declines gradually until it reaches <10 ug/dl in the evening (6-8pm).[6]
The 24-hour Urine free cortisol (UFC) excretion is elevated > 120 µg/24h (>331 nmol/24h) in patients with cushing’s disease. The normal value ranges between 20 to 100 µg/24h ; Moreover, The 24-hour Urine free cortisol excretion is also increased < 150 µg/24h in obese patients.[35][36][37]
The amount of cortisol in blood over a period of 24 hours is greater than 100 micrograms.[1][38]
Dexamethasone suppression test, to test cortisol secretion after shutting down steroid production in the adrenal gland by administering 1 mg of dexamethasone by mouth (per os) at mid night, and measuring plasma cortisol level the next morning (7-8 am), it will clear if the case is Acth dependent or not. Normally, in healthy people suppression of morning plasma cortisol to less than 5 ug/dl is observed; however, in patients with cushing’s syndrome the level of cortisol is equal to or greater than 9 ug/dl, while preserving plasma cortisol level at its initial level. Furthermore, CT imaging or MRI of the adrenal glands will be made to search for tumors; however, CT imaging or MRI of the brain and chest must be made if a pituitary tumor is suspected (by origins).
Blood analysis
The symptoms of decreased potassium are nonspecific, and the condition is usually discovered in a blood test, which reveals decreased serum K levels. Normal serum potassium levels range between 3.5 and 5.0 mEq
Giving oral dexamethasone 0.5 mg q 6 h (every 6 hours) for 2 days to healthy people leads to inhibition of ACTH secretion in the pituitary, causing a drop in the urinary free cortisol level to less than 10 µg/24h on the 2nd day; however, in patients with Cushing’s disease, pituitary ACTH secretion is relatively resistant to suppression, and urinary free cortisol level will not decrease in a normal fashion, but when the oral dose of dexamethasone is increased to 2 mg q6h for two successive days (high dose), urinary-free cortisol will usually decrease by at least 50% from the baseline values in patients with Cushing’s disease, which is dependent on pituitary ACTH.[51]
In patients with adrenal tumors, dexamethasone will have no suppressive effects because cortisol production is independent of ACTH; however, in patients with ectopic ACTH syndrome, the production of ACTH by nonpituitary tumor is almost always unaffected by dexamethasone, hence urinary steroids remain unchanged.
The dexamethasone test distinguishes Cushing’s syndrome from other pituitary disorders.
A more precise variant is to give dexamethasone 1 mg/hr by continuous IV infusion for 7 hours. The plasma cortisol level decreases by at least 7 mg/dL or more after seven hours; however, patients with adrenal tumors or the ectopic ACTH syndrome do not respond.[48][49][50]
*Dexamethasone suppression is blocked by rifampicin, so tests of this type are useless and of no point in patients receiving this drug.
The overnight metyrapone test is used to determine the etiology of Cushing’s syndrome, as metyrapone blocks the 11-hydroxylation of cortisol from 11-deoxycortisol . Patients with pituitary dependent Cushing’s disease show a marked increase in plasma 11-deoxycortisol, but serum 11-deoxycortisol levels will not increase in patients with adrenal tumors or ectopic ACTH syndrome. The total amount of steroids produced (total cortisol and 11-deoxycortisol) is measured to rule out whether an increase in total steroids level has occurred.[45][46][47]
ACTH stimulation test is less useful for evaluating Cushing’s syndrome. 50 U of ACTH are infused continuously i.v. over an 8-h period, which can lead to a two-to-five fold increase in urinary cortisol level in patients with Cushing’s disease, especially those suffering of bilateral hyperplasia and hyper responsiveness due to chronic endogenous ACTH excess. In about half of patients with adrenal adenoma, ACTH stimulation produced a clear and sometimes marked increase in plasma and urinary cortisol; however, Adrenal carcinomas are generally unresponsive to ACTH.[42][43][44]
MRI is more useful than CT in imaging pituitary microadenomas, especially with a high resolution technique augmented by gadolinium. However, some microadenomas are difficult to visualize even with all these advanced modalities. In some cases, studies found no abnormality in the pituitary despite clear evidence of ACTH over production.[39][40][41]
Causes and Treatment
References
- emc.healthyorthodoxmedicine.com
- nlm.nih.gov/medlineplus/ency/article/000410.htm
- pituitary.mgh.harvard.edu/CushingsSyndrome.htm
- cdc.gov/healthyweight/calories/other_factors.html
- aafp.org/afp/2000/0901/p1119.html
- nejm.org/doi/pdf/10.1056/NEJM198605223142101
- merckmanuals.com/professional/endocrine-and-metabolic-disorders/adrenal-disorders/cushing-syndrome
- endocrine-abstracts.org/ea/0029/ea0029p953.htm
- ncbi.nlm.nih.gov/pmc/articles/PMC3002408/
- aafp.org/afp/2003/0615/p2565.html
- ncbi.nlm.nih.gov/pubmed/9648484
- annals.org/article.aspx?articleid=677461
- ncbi.nlm.nih.gov/pubmed/20829620
- nhs.uk/Conditions/Cushings-syndrome/Pages/Symptoms.aspx
- ncbi.nlm.nih.gov/pubmed/12727957
- cedars-sinai.edu/Patients/Health-Conditions/Cushings-Syndrome.aspx
- ncbi.nlm.nih.gov/pubmed/9745407
- press.endocrine.org/doi/pdf/10.1210/jcem.83.9.5084
- nature.com/nrendo/journal/v3/n11/full/ncpendmet0665.html
- ncbi.nlm.nih.gov/pmc/articles/PMC2772220/
- imperial.edu/admin/Media/File_Upload/155-Files/NS211/Cushings syndrome.pdf
- journals.lww.com/psychosomaticmedicine/Abstract/1953/07000/Psychotic_Reactions_Induced_by_Corticotropin.2.aspx
- books.google.co.uk/books?isbn=1300443049
- pituitary.org.uk/information/symptoms,-diagnosis-and-tests/symptoms/
- jpbjournal.com/admin/fckeditor/_samples/php/article/106_18-21.pdf
- ncbi.nlm.nih.gov/pubmed/1879061
- ncbi.nlm.nih.gov/pubmed/3525245
- ncbi.nlm.nih.gov/pubmed/8651039
- pituitary.ucla.edu/cushings-disease
- niddk.nih.gov/health-information/health-topics/endocrine/cushings-syndrome/Pages/fact-sheet.aspx
- nlm.nih.gov/medlineplus/ency/article/000407.htm
- columbiasurgery.org/conditions-and-treatments/cushings-syndrome
- my.clevelandclinic.org/health/diseases_conditions/hic-Overactive-Pituitary-Gland-Hyperpituitarism
- hopkinsmedicine.org/healthlibrary/conditions/endocrinology/overactive_adrenal_glandscushings_syndrome_85,P00403/
- med.stanford.edu/neurosurgery/pituitary/cushings_syndrome.html
- acb.org.uk/Nat Lab Med Hbk/Cortisol Urine.pdf
- urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=167&ContentID=cortisol_urine
- us.corwin.com/sites/default/files/upm-binaries/17430_Chapter_3.pdf
- ncbi.nlm.nih.gov/pmc/articles/PMC3183511/
- cancer.org/cancer/pituitarytumors/detailedguide/pituitary-tumors-diagnosis
- pituitary.ucla.edu/pituitary-adenomas
- ncbi.nlm.nih.gov/pmc/articles/PMC3860097/
- jci.org/articles/view/103028/version/1/pdf/render
- press.endocrine.org/doi/pdf/10.1210/jcem.83.10.5156
- ncbi.nlm.nih.gov/pubmed/225638
- ncbi.nlm.nih.gov/pmc/articles/PMC4215264/
- nhs.uk/Conditions/Cushings-syndrome/Pages/Diagnosis.aspx
- ncbi.nlm.nih.gov/pubmed/3402181
- ncbi.nlm.nih.gov/pubmed/9645457
- drugs.com/dosage/dexamethasone.html
- globalrph.com/dexamethasone_dilution.htm
How to Diagnose Cushings syndrome
Verified by: Dr.Diab (January 7, 2017)
Citation: Dr.Diab. (January 7, 2017). How to Diagnose Cushings syndrome. Medcoi Journal of Medicine, 32(2). urn:medcoi:article4363.













There are no comments yet
Or use one of these social networks