How to Treat Cushings Disease
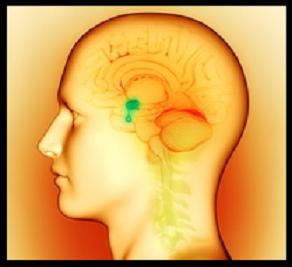
Cushings syndrome (ectopic Acth syndrome) is a pituitary-dependent adrenal disorder caused by overactive adrenal tumors, it is characterized by hypercortisolism, which is a condition of biochemical cortisol excess. Less commonly, Bilateral ACTH-independent macronodular adrenocortical hyperplasia (AIMAH) may lead to Cushing syndrome. [2][3][4]
Cortisol production is regulated by pituitary Acth (adrenocorticotropic hormone).
Causes of excess cortisol production:
(1)– Cushings disease (Pituitary tumor), it accounts for 60% of the cases. Characteristic diagnostic findings in Cushing’s disease include increased plasma cortisol and ACTH levels.
(2)– Adrenal tumor is the second most common cause of hypercortisolism, it is characterized by increased plasma cortisol levels and decreased serum ACTH levels, as hypercortisolism may suppress ACTH production.
- Adrenal adenoma accounts for about 25% of the cases.
- Adrenal carcinoma, is a rare form of cancer in the outer layer of the adrenal gland, it accounts for about 10% of the cases, letrogenic steroids.
(3)– Ectopic Cushing syndrome, is a form of Cushing syndrome in which adrenocorticotropic hormone (ACTH) is produced in a tumor outside the pituitary gland, such as in the case of lung cancers, it accounts for about 5% of the cases.

How to treat cushing’s disease
Understanding the condition
The precise treatment of Cushing’s Disease will vary depending on the cause; however, it involves controlling the adrenal or pituitary tumors and regulating the hyperactivity of the pituitary, which in turn controls the functions of most other endocrine glands.
Clinical management of Cushings disease
The initial workup for cushing’s syndrome consists of a supportive therapy to maintain the patient’s condition while physicians treat the underlying causes, conventional drugs can also be used to treat the symptoms. Typically appropriate amounts of dietary Proteins (HP) and vitamin K (phylloquinone) are administered to all critically ill patients if the clinical picture is severe, especially when patients suffer complex problems presenting in a diverse array of clinical symptoms such as:
Hypokalemia (hypokalaemia) is a condition in which blood potassium level is lower than normal due to severe metabolic disturbances caused by Adrenocortical hyperfunction.
Hyperglycemia or high blood sugar is a condition in which an excessive amount of plasma glucose circulates in the blood, normal plasma glucose level ranges between 60 and 100 mg/dl.
Hypertension or high blood pressure (HBP), is a condition in which the arterial blood pressure is persistently peaking above 150 mmHg, a blood pressure level between 140 and 150 mmHg is called prehypertension. Normal blood pressure level ranges between 80-110 mmHg for women and 90-120 mmHg for men.
Renal colic is an acute phase of abdominal pain caused by kidney stones. Hypertension or high blood pressure may contribute to worsening abdominal pain. It may be necessary to block steroid secretion if the disease is caused by adrenal tumor, cortisol secretion can be blocked by oral administration of anti-steroid drugs such as Aminoglutethimide (Cytadren) which acts on the adrenal cortex and suppresses production of steroids, 250 mg po bid is the usual adult dose for cushings syndrome. ketoconazole is an effective drug for long term control of hypercortisolism, usual adult dose involves oral administration of 400 to 1200 mg of ketoconazole daily. [5]
Transsphenoidal exploration of the pituitary is a standard approach performed to all patients suffering of Pituitary ACTH hypersecretion to seek pituitary tumors, adenomectomy (a surgical procedure) is performed if extensive pituitary exploration reveals an adenoma (a tumor), The success rate for this treatment option decreases from 70% depending on the size of the tumor, good results can be achieved for microadenomas (tumors less than 1 cm in diameter). This operation is not contraindicated in pregnancy. Moreover, approximately 20% of patients with large tumors will suffer of early tumor recurrence.
Supervoltage or proton beam irradiation of the pituitary gland can be used to treat pituitary tumors and acromegaly. Supervoltage beam radiation is delivered using high energy X-ray machines, an X-ray beam at a total dose of 50 Gy reduces the secretion of ACTH (adreno corticotropin hormone). Irradiation with heavy particle beam at a total dose of 100 Gy is also successful. Response to irradiation may require several weeks or months.
Pituitary irradiation may be contradicted in children because irradiation may cause unwanted side effects. However, irradiation may reduce the secretion of growth hormone causing precocious puberty.
Bilateral adrenalectomy is performed for patients with pituitary hyperadrenocorticism who do not respond to both pituitary exploration and irradiation, this treatment requires a lifelong steroid replacement therapy; Moreover, steroid replacement therapy is also required for the treatment of primary adrenal failure.
Treatment of pituitary tumors can be achieved by surgical removal of the tumor followed by radiation therapy of the pituitary.
Adrenocortical tumors are surgically removed and patients are given supplementary cortisol during the operation; however, the treatment is lifelong steroids, especially in the postoperative periods because of adrenocortical atrophy and glandular adrenal insufficiency (suppressed cortisol production and cortisol deficiency).
Laparoscopic adrenal ectomy is performed if diagnostics show a well defined small tumor (benign adenoma or non cancerous tumor) whereas bilateral adrenalectomy may be necessary to treat multinodular adrenal hyperplasia (multi tumor nodes).
Plan treatment of the ectopic ACTH syndrome where ACTH is secreted in tumor cells outside the pituitary, especially in some forms of lung cancer consists of removing the ectopic acth producing tumors; However, this procedure is not practical because in most cases the tumor is disseminated (spread all over the tissue) and cannot be excised.
Severe metabolic disorders such as hypokalemia are best controlled by adrenal inhibitors, metyrapone is a drug of choice often used in the diagnosis of adrenal insufficiency, usual adult dose involves oral administration of metyrapone at a dose of 250 mg per day with aminoglutethimide at a dose of 250 mg orally twice a day, the maximum dose can be individually increased to suit the patients demands; however, the maximum dose should not exceed 2 g/day. Alternatively, Mitotane or Lysodren blocks hormone production in the adrenals, but it should be used cautiously due to liver toxicity, optimal dosage includes oral administration of 0.5 g Mitotane per day, the dose can be individually increased to a maximum total dose of 8 to 12 g/day. Adrenocortical hyperactivity can be controlled by a combination of mitotane (8-12 g/day) and cortisol (20 mg/day).
Ketoconazole best blocks steroid synthesis; however, it should be used cautiously due to liver toxicity and because it has the potential to trigger signs and symptoms of Addison’s disease such as depression, weakness, darkened skin, low blood pressure, decreased serum sodium, increased serum potassium and increased serum calcium.[6][7]
Alternatively, mifepristone (RU 486) is a drug often used with misoprostol to induce an abortion; however, it is also used to control steroid side effects because it has the potential to block the corticosteroid receptors. Mifepristone should be used cautiously because it raises the plasma cortisol level.[18][19][20]
Ectopic ACTH syndrome responds to long-acting somatostatin analogs, octreotide (Sandostatin or Octreotide Acetate) is an injectable somatostatin analogue that inhibits growth hormone, glucagon, and insulin. It is normally used for the treatment of Ectopic ACTH syndrome (EAS), acromegaly and many other endocrine disorders, the starting dose ranges from 100 to 125 mg given subcutaneous (sc) 3 times a day (tid) for periods longer than 2 years. Octreotide should be administered cautiously because chronic (long-term) use is often associated with several complications such as mild gastritis (inflammation of the gastric mucosa), which may cause symptoms like nausea, vomiting, and epigastric discomfort; gastritis can be treated by:[16][17]
- Antacids, are drugs that neutralize the gastric acid by raising the gastric pH. Maalox Antacid is a popular drug used as symptomatic relief of heartburn, dyspepsia, or stomach upset and to protect the gastric mucosa from acidic gastric juices (hydrochloric acid and noxious agents).
- H2 blockers. are a group of drugs used to reduce the amount of acid produced by the epithelial cells of the stomach, so they are used to prevent acidic damage on the inflamed mucosa. Ranitidine is a popular drug used to relieve symptoms of acid reflux, or gastroesophageal reflux disease (GERD).
- Proton pump inhibitors (PPIs), are a group of drugs used to reduce the amount of acid produced by the epithelial cells of the stomach. Omeprazole is a popular drug often used to treat gastric acidity and to relieve symptoms of gastroesophageal reflux disease, etc.[14][15]
Dietary guidelines for cushing’s syndrome
Cushing’s syndrome may require special dietary changes, especially that it may cause weight gain, fatigue, skin changes and depression. Low-sodium, fat free meals are highly recommended, healthy eating starts with a DASH diet, a proper heart healthy diet starts by consuming enough amounts of unsaturated fats such as fish oil and olive oil, decrease the amount of processed foods you eat, and stop eating junk food for good, reduce eating fast food and stop eating fried foods, maintain a healthy low sugar diet based on carbohydrates (rice, potatoes, whole grain), avoid overeating laxative green vegetables such as lettuce or cabbage because they increase the acidity of the stomach, especially if you eat them raw and in big quantities without bread.[8][9]
- Drink parsley tea or green mint tea on regular basis may play an important role in the prevention of gallstones.
- Jaundice (icterus), is a yellowish discoloration of the skin due to high bilirubin levels, it is frequently associated with cirrhosis, cholelithiasis or pancreatic disease; however, natural jaundice can be cured within few weeks by diet therapy, drink a liter of grapefruit juice per day, and keep on this regimen until achieving a full cure of jaundice; However
, precautions can be made to minimize the risk of developing natural jaundice, start your day by drinking a cup of grapefruit juice on an empty stomach, and keep on this regimen for three consecutive months. - B12 deficiency (hypocobalaminemia) and malabsorption of vitamin B12 is common especially if you have atrophic gastritis. Vitamin B12 deficiency is usually treated with injections of hydroxocobalamin (vitamin B12 supplement).[10]
Notice: increased serum cortisol can be a sign of liver disease, when the hepatocytes or liver cells lose the ability to oxidize cortisol into cortisone (an inactive metabolite of cortisol); however, in this case the levels of ACTH and cortisol in the blood are both increased because of the reduced sensitivity of the hypothalamic-pituitary system to the feedback mechanisms of the principal hormones, Normally, increased plasma cortisol levels should reduce ACTH secretion.
Chronic liver disease is is often caused by chronic alcoholism and malnutrition. Treatment can be made by improving the liver function, blockers of corticosteroid activity such as ketoconazole are recommended. The optimal starting dose of ketoconazole ranges from 400 to 1200 mg/day.[11][12][13]
References
- emc.healthyorthodoxmedicine
- press.endocrine.org/doi/full/10.1210/jc.2009-0881
- orpha.net/consor/cgi-bin/OC_Exp.php?Lng=EN&Expert=189427
- ojrd.biomedcentral.com/articles/10.1186/1750-1172-8-142
- drugs.com/dosage/aminoglutethimide.html
- ncbi.nlm.nih.gov/pubmed/3023421
- ncbi.nlm.nih.gov/pubmed/24471573
- medcoi.com/health/heart-healthy-diet/
- medcoi.com/health/nephrosclerosis/#prevention
- ncbi.nlm.nih.gov/pubmed/3604755
- .edmcasereports.com/articles/endocrinology-diabetes-and-metabolism-case-reports/10.1530/EDM-14-0083
- ncbi.nlm.nih.gov/pmc/articles/PMC4256723/
- ncbi.nlm.nih.gov/pmc/articles/PMC3273924/
- ncbi.nlm.nih.gov/pmc/articles/PMC2266058/
- drugs.com/health-guide/gastritis.html
- pmj.bmj.com/content/75/880/65.full
- ncbi.nlm.nih.gov/pmc/articles/PMC3683198/
- ncbi.nlm.nih.gov/pubmed/17984235
- ncbi.nlm.nih.gov/pubmed/8734015
- ncbi.nlm.nih.gov/pmc/articles/PMC3944746/
How to Treat Cushings Disease
Verified by: Dr.Diab (January 7, 2017)
Citation: Dr.Diab. (January 7, 2017). How to Treat Cushings Disease. Medcoi Journal of Medicine, 17(2). urn:medcoi:article4370.













There are no comments yet
Or use one of these social networks