Proctitis Types Symptoms Causes Diagnosis and Treatment
What is Proctitis?
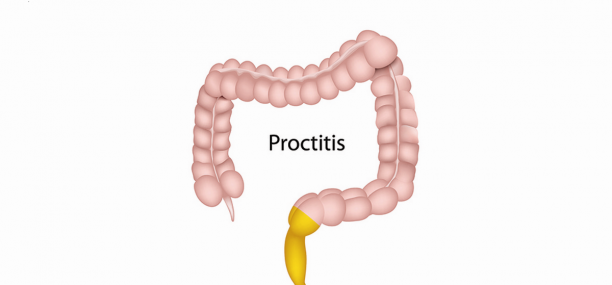
Proctitis (проктит, التهاب المستقيم) is a medical term used to describe an inflammation of the rectal lining that usually causes proctalgia fugax (rectal pain) and tenesmus (continuous sensation that you need to have a bowel movement).
The rectum is a muscular tube through which wastes are eliminated, it connects the anus to the end of your colon.
What are the different types of proctitis?
There are four main types of proctitis:
1- Diversion Proctitis or Nonspecific Proctitis
2- Distal Proctitis or Common Proctitis
3- Radiation Proctitis
4- Ulcerative Proctitis or Idiopathic Proctitis
What is diversion proctitis?
Diversion colitis or diversion proctitis is a nonspecific inflammatory disorder that occurs in rectal segments that are surgically diverted from the faecal stream such as in the case of creating a loop colostomy /ileostomy or an end ileostomy /colostomy with closure of the distal colon segment (Hartmann’s procedure, which is a surgical procedure that involves resection of the rectosigmoid colon with with closure of the anorectal stump and formation of an end colostomy).
What is distal proctitis?
Distal proctitis is a form of rectal inflammation affecting the lining of the rectum that begins at the rectum and extends up through the lower part of the colon. It causes tenesmus, pain, irritation, ulcerations or sores and a discharge of blood, mucus or pus.
The colon is the end of the large intestine.
What is radiation proctitis?
Radiation proctitis is a form of radiation colitis affecting the lower part of the colon. It is characterized by inflammation and damage to the lower parts of the colon that arises after exposure to x-rays or other ionizing radiation therapies.
What is idiopathic proctitis?
Ulcerative proctitis is an idiopathic inflammatory form of ulcerative colitis involving only the mucosal folds of the rectum and is therefore an anatomically limited form of idiopathic inflammatory bowel disease.
Is ulcerative proctitis serious?
Ulcerative proctitis is rarely serious though it can be painful and unsettling. However, about one third of patients with ulcerative proctitis eventually develop ulcerative colitis, which has more severe symptoms and affects the entire colon.
What is rectal lining inflammation?
Both ulcerative colitis and Crohn’s disease can cause proctitis. These two forms of inflammatory bowel disease often cause irritation and sores in the inner lining of the colon and rectum.
Can you get cancer from ulcerative colitis?
Ulcerative colitis is a lifelong inflammatory bowel disease (currently there is no cure for it). However, proper control management and medications can improve symptoms and surgery can also help in many cases when all other drugs have proved ineffective. Moreover, it is important to mention that people with ulcerative colitis have an increased risk of developing colorectal cancer and should be monitored regularly, especially those patients with chronic severe ulcerative colitis.
What are the symptoms of proctitis?
Common symptoms and signs of Proctitis include:
- Tenesmus or feeling an urge to defecate (feeling that you need to have a bowel movement).
- Rectal bleeding and Hematochezia (bloody bowel movements).
- Pus-like rectal discharge (the passing of mucus or pus through your rectum).
- Proctalgia or rectal pain.
- Abdominal colic or severe spasmodic pain that is felt mainly the left side of your abdomen (crampy abdominal pain).
- Pain with bowel movements.
- A feeling of rectal fullness.
- Diarrhea or frequent passage of loose or liquid stools.
What are the causes of proctitis?
Common causes of proctitis include:
- Sexually transmitted infections (STIs)
- Inflammatory bowel disease (IBD), such as ulcerative or Crohn’s disease.
- Anal trauma, such as having anal sex.
- Antibiotic-associated colitis and rectal infections that occur after antibiotic use, such as clostridium difficile infection (C. difficile or C. diff infection).
- Bacterial infections that aren’t sexually transmitted, such as salmonella or shigella, etc.
What causes ulcerative proctitis?
Ulcerative proctitis is an idiopathic inflammatory form of ulcerative colitis involving only the mucosal folds of the rectum, and is therefore characterized by fine ulcerations in the rectal mucosa that do not penetrate the rectal muscle wall.
Can proctitis be caused by stress?
Although the cause of ulcerative proctitis is not identified, it is known that stress do not cause it. However, stress aggravates the symptoms of ulcerative proctitis, and thus managing stress levels may reduce the severity of symptoms.
What causes rectal pain after bowel movement?
An anal fissure is a small crack in the anal lining that may occur when passing large hard stools, or straining during delivery. Anal fissures can cause proctalgia and bleeding during and after defecation. Moreover, it may also cause anal itching and burning sensation around the anus.
How to diagnose proctitis?
Diagnosis is made based on:
- Clinical presentation.
- Endoscopic findings (endoscopic appearance).
- histopathology.
Tests and procedures used to diagnose proctitis include:
Blood tests to detect blood loss, tumors or infections.
Stool test, a stool test can show signs of rectal bleeding and signs of possible infections that may cause proctitis to ruleout if your proctitis is caused by a bacterial infection.
Faecal occult blood test, the faecal occult blood test helps to diagnose lower gastrointestinal bleeding.
Colonoscopy of the colon allows your doctor to look at the inner lining of your rectum and colon to rule out sores, tumors, polyps and areas of inflammation or bleeding (bowel scope screening).
Flexible sigmoidoscopy, a flexible sigmoidoscopy is used to examine and evaluate the rectum and the lower part of the colon, it usually lasts from 10 to 20 min.
CT Evaluation of the Colon, CT of the abdomen and pelvis with iv contrast is widely used to assess patients who are suspected of having proctitis or colitis.
Testing for sexually transmitted infections, faecal analysis and stool culture to find out if bacteria may be causing proctitis.
What does it mean when you have white blood cells in your stool?
Leukocytes (white blood cells) are immune cells that can show up in the stool if you have inflammatory bowel disease such as an inflammatory diarrhea. This type of presence may be a sign of an infection caused by bacteria such as shigella, salmonella, clostridium difficile, or campylobacter, etc.
How to treat proctitis?
Treatment may include:
1- Anti-inflammatory medications to control rectal inflammation (either by mouth or as a suppository or enema). Your doctor may prescribe drugs such as mesalamine (mesalazine, INN, BAN, Asacol, Canasa, USAN, 5-aminosalicylic acid, 5-ASA, etc.), or corticosteroids such as Rayos (prednisone) or budesonide (Entocort EC, Uceris, etc.).
2- Antidiarrheal medicines to stop diarrhea such as Imodium (loperamide) and bismuth subsalicylate (Kaopectate, Pepto-Bismol).
3-Surgery to remove the diseased part of the colon. However, surgery is rarely indicated for proctitis secondary to infections.
A doctor may prescribe metronidazole (Flagyl) or vancomycin (Vancocin) to treat Proctitis caused by antibiotics.
Ganaton 50 mg (Itopride, INN) and Trimedat 150 mg (Trimebutine Maleate) are used to control IBS.
References
Verified by: Dr.Diab (November 1, 2017)
Citation: Dr.Diab. (November 1, 2017). Proctitis Types Symptoms Causes Diagnosis and Treatment. Medcoi Journal of Medicine, 16(2). urn:medcoi:article17986.











There are no comments yet
Or use one of these social networks