Uterine Fibroids
What are uterine fibroids made of?
Uterine fibroids (Leiomyomas or myomas) are benign uterine tumors of smooth muscle origin (smooth-muscle tumors), these tumors can grow quite large and may cause severe abdominal pain and heavy periods; however, most women with uterine fibroids are asymptomatic (have no symptoms).
How common are uterine fibroids?
Uterine fibroid tumors are the most common pelvic neoplasms that occur more often in black women than in white women, uterine fibroids occurrence rate for adult women was 66% higher for Black women than white women (5 to 3). However, nearly 50% of women have fibroids by age 50.
Uterine fibroids affect women of all backgrounds, regardless of gender, race or ethnicity, although African Americans and Hispanics report the condition more often than Caucasians. Uterine fibroids are rare in women under age 20.
Types
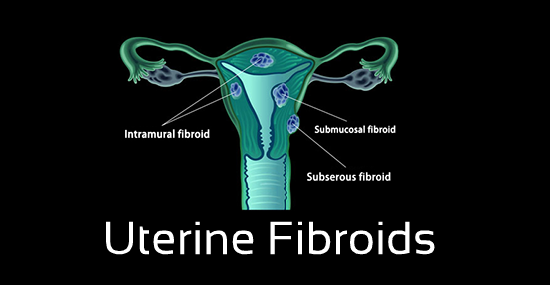
What are the different types of uterine fibroids?
Fibroids can be divided into four different types:
- Submucosal fibroids are benign neoplasms that grow into the uterine cavity (into the endometrium). Submucosal fibroids decrease fertility; However, their removal restores fertility to baseline rates.
- Intramural fibroids are benign neoplasms that grow within the myometrium (muscular uterine wall).
- Subserosal fibroids are benign neoplasms extending outside the uterus into the pelvis, they project to the outside of the uterus (grow on the outside of the serosa).
- Pedunculated uterine fibroids are benign neoplasms that grow on a stalk, resulting in pedunculated subserosal fibroids (extending outside the uterus into the pelvis on a stalk) or pedunculated submucosal (grow into the uterus on a stalk).

How large can a fibroid grow?
Uterine fibroids can range in size from a quarter of an inch (0.6 centimeters) to larger than a cantaloupe (12 cm).
Characteristics
Do fibroid tumors go away after menopause and what is the cause of uterine fibroids?
Fibroids are usually multiple monoclonal neoplasms (arising from a single smooth muscle cell) with estrogen receptors (ER), which means that they can increase in size during reproductive years and usually regress after menopause.
What causes fibroids to grow rapidly?
In most cases, uterine fibroids grow rapidly during the first and second trimesters of pregnancy, when hormone (estrogen and progesterone) levels are high.
Where do fibroid tumors develop?
Most fibroids grow in the wall of the uterus; however, they may have significant negative impact on a woman’s quality of life, as they can cause significant morbidity.
What are the complications of uterine fibroids?
Large or rapidly growing fibroids can lead to compromised endometrial perfusion, which, in turn, can cause consistent lower abdominal pain and swelling.
What is degeneration of fibroids and what is meant by benign degeneration of fibroids?
Benign degeneration occurs when a fibroid grows so fast that the central areas may not receive an adequate blood supply. Benign degeneration is often followed by calcification; however, the loss of blood supply may result in different types of degeneration.
What are the different types of fibroid degeneration?
Uterine fibroids can undergo several types of degeneration. The five main types of degeneration that can involve a uterine leiomyoma are: hyaline degeneration, cystic degeneration, myxoid degeneration, calcific degeneration, and red/carneous degeneration.
What is hyaline degeneration of fibroids?
Hyaline degeneration of a leiomyoma (focal or generalized hyalinization) is the most common form of degeneration characterized by transparent or glassy masses (rounded masses or broad bands) of homogeneous acidophilic substances, this type accounts for more than 60% of all cases.
What is myxoid degeneration of fibroids?
Myxoid degeneration of a leiomyoma (myxoid uterine leiomyoma or myxomatous degeneration) is a rare type of degeneration characterized by complex cystic masses filled with a gelatinous material (it contains jelly like myxomatous connective tissue).
What is a calcified uterine fibroid?
Calcific degeneration is the end stage of the degenerative process, which is characterized by calcium deposits that develop on the remaining fibroid tissue. It accounts for approximately 4% of all cases.
What is a cystic uterine fibroid?
Cystic degeneration (cystic adenomyoma of the uterus) is a relatively common, benign uterine pathology commonly seen in middle aged women, it is characterized by the presence of myometrial cysts, cystic lesions are described as round, well-demarcated fluid-filled sacs.
What is red degeneration of fibroids?
Red degeneration occurs most often during pregnancy and is also associated with use of oral contraceptives or it can be caused by necrosis due to impaired blood supply, it is a hemorrhagic infarction caused by insufficient blood flow to the center of the lesion, the patient often presents with an acute abdomen.
Ultrasound scans are recommended in the early pregnancy to identify those fibroids that can cause significant symptoms and clinical problems due to their size and location.
Symptoms
What are the symptoms of uterine fibroids?
In most cases, fibroids do not cause any symptoms. However, in symptomatic women with uterine fibroids, the most common symptoms include:
- Menorrhagia or abnormal menstrual periods with heavy or prolonged bleeding (abnormal profuse menstrual flow).
- Menometrorrhagia or abnormal menstrual periods with prolonged or excessive uterine bleeding that occur irregularly and more frequently than normal. It is thus a combination of menorrhagia and metrorrhagia.
- Intermenstrual bleeding or abnormal bleeding between menstrual periods
- Severe abdominal pressure and pain
- Urinary bowel problems such as frequency, urgency and constipation
- Recurrent abortions
- Infertility
- Palpable masses
Premature labor (Premature contractions or preterm labor) remains the main complain during pregnancy that necessitates a C-section (cesarean section).
Diagnosis
How to diagnose uterine fibroids?
A pelvic examination (vaginal examination) is a visual inspection of a woman’s pelvic organs. This physical examination helps in evaluating the size and position of the vulva, vagina, cervix, uterus, and ovaries.
An ultrasound is the best test to confirm Uterine fibroids; however, abdominal ultrasound should always be repeated after 4-6 months to check the fibroid’s growth and to determine whether the fibroid is growing rapidly.
Treatment
How to treat uterine fibroids?
Treating asymptomatic patients is not indicated.
Progestin-Only birth control pills, contraceptive hormones that block ovulation through suppression of ovarian function can also be used to stop bleeding associated with uterine fibroids.
Estrogen suppression is often used to stop bleeding, lack of estrogen can also induce infertility by preventing ovulation.
GnRH agonists are commonly given preoperatively to manage anemia and reduce the size of fibroids.
Exogenous progestins: medroxyprogesterone acetat 5-10 mg/dl PO 10-14 days per menstrual cycle – this treatment is used to treat and prevent bleeding, it reduces bleeding after 1-2 cycles; Continuous daily treatment decreases bleeding; however, medicines, such as medroxyprogesterone acetat, sometimes cause spotting between periods (abnormal vaginal bleeding) due to hormonal imbalances.
Depot medroxyprogesterone acetat 150 mg IM for 3 months is an injectable contraceptive (progestin-only) that controls bleeding and prevents contraception, this method of contraception (birth control) is 100% effective; Adverse affects include weight gain, depression and irregular bleeding.
Surgical options include myomectomy and hysterectomy
References
Verified by: Dr.Diab (November 7, 2017)
Citation: Dr.Diab. (November 7, 2017). Uterine Fibroids Types Symptoms and Treatment. Medcoi Journal of Medicine, 20(2). urn:medcoi:article3219.












There are no comments yet
Or use one of these social networks