Chronic Anovulation Causes Symptoms and Treatment
What is Chronic Anovulation?
Chronic anovulation (ановуляция) is the most common form of amenorrhea or the absence of menstruation either because it never started or later ceased, it is characterized by low to normal levels of gonadotropins, relative hypoestrogenism and irregular, profuse uterine bleeding. It usually occurs as a result of unopposed estrogenic stimulation among non-pregnant women of reproductive age (both girls and sexually active women can be effected). In most cases, anovulation is caused by abnormal gonadotropin secretion due to a functional derangement of the hypothalamo-pituitary system consequent to inappropriate estrogen feedback.
Anovulation is the most common cause of oligomenorrhea or amenorrhea in women of childbearing age
Anovulation often occur due to abnormalities in the hypothalamic-pituitary-adrenal (HPA) axis, such as inappropriate hormonal feedback. Evidence suggests that the hypothalamic form is a heterogeneous group of disorders that produce similar clinical manifestations and to which body composition, stress, diet, exercise, environment, genetic background, and other unknown factors contribute in varying degrees.
Inappropriate hormonal feedback may result from functional abnormalities and disorders, such as abnormal sex hormone binding globulin, obesity, low SHBG levels, liver disease, polycystic ovary syndrome (PCOS), functional androgen excess (hyperandrogenism), and other endocrine disorders
The role of adrenal hyperandrogenism, SHBG, PCOS, obesity and insulin resistance in anovulation
Abnormal sex hormone binding globulin or low SHBG levels. Sex hormone binding globulin (SHBG, or SSBG) is a blood glycoprotein that transports androgen and estrogen (testosterone and estradiol) in plasma and regulates their availability to target cells. Sex hormone-binding globulins are synthesized in the liver. The levels of SHBG are regulated by several hormones. Testosterone and insulin inhibit SHBG synthesis whereas estrogen and thyroid hormone stimulate its production.
SHBG binds androgen and estrogen and decreases their biologic activities
Abnormal sex hormone binding globulins are commonly associated with liver disease, whereas, low SHBG levels are associated with lifestyle choices, obesity, stress, polycystic ovary syndrome (PCOS), exogenous androgens (increased circulating levels of testosterone), increased growth hormone levels (high GH values), high fasting insulin levels (increased insulin levels in blood), and liver diseases, such as hepatitis, alcoholic fatty liver disease, cirrhosis, and liver cancer.
In women with PCOS, circulating levels of SHBG are reduced by approximately half. Insulin directly decreases serum SHBG levels and increases free testosterone levels by suppressing SHBG and increasing ovarian secretion of testosterone.
In patients with diabetes mellitus, SHBG is usually low, and for this reason low SHBG levels suggest insulin resistance and diabetes
High SHBG levels are often associated with high cortisol. Free testosterone levels decreased as concentrations of cortisol increased in early morning. Cortisol is an adrenal steroid hormone released in response to stress and low blood glucose levels. High cortisol levels can increase your body fat and decrease your ability to lose weight.
In patients with stress, SHBG is usually elevated
Normally, SHBG buffers major fluctuations in the plasma levels of steroids, as it is a major carrier of androgens. Approximately two-thirds of testosterone is bound to sex hormone binding globulin (SHBG), whereas about one-third is bound to albumin
The role of obesity in anovulation
Obese women have an increased tendency to develop diabetes. Moreover, being overweight or obese increases the risk of hypertension and strokes.
Normal body fat percentage for women ranges between 20 and 30. However, your estrogen levels begin to increase when body fat increases above 20% and the more you gain weight the more estrogen you will have, as extra body fat contributes to excessive extraglandular production of estrogen
Androgen excess (hyperandrogenism) is usually caused by an ovarian or adrenal pathology. In females, androgen excess is characterized by excessive levels of testosterone
What are the signs of low SHBG in women?
Signs of low SHBG in women include:
- Hyperandrogenism or high levels of androgens due to ovarian overproduction of androgens (testosterone), which is common in women with ovarian tumors and polycystic ovary syndrome (PCOS)
- Hirsutism (male pattern hair growth) or androgenetic alopecia (male pattern hair loss, MPHL)
- Menstrual irregularities (missed or irregular periods)
- Changes in the breasts (insufficient glandular tissue or breast hypoplasia) due to reduced estrogen
- Skin abnormalities, such as eczema or atopic dermatitis
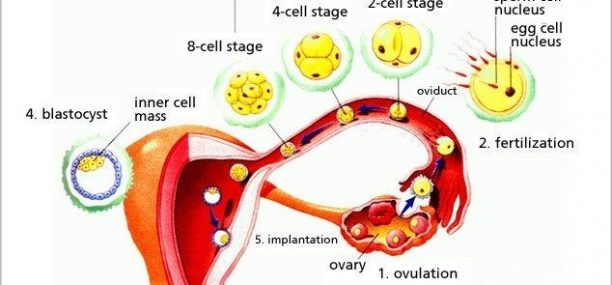
Chronic anovulation is defined as a prolonged abnormal phase in which cyclic ovulation is impaired due to abnormalities in the hypothalamic-pituitary-adrenal (HPA) axis, this happens when the ovary (the target organ) does not receive the necessary stimulatory signals, and as a result, ovulation and menstruation do not occur.
In most cases, no anatomic abnormalities of the target organs prevent menstruation from coming, and for this reason, ovulation can be induced or re-initiated with proper management because the function of the ovarian follicles remains intact.
Symptoms
What are the symptoms of chronic anovulation?
In most cases, alteration of menstrual cycle is the primary symptom of chronic anovulation. For most women, anovulatory menstrual periods are characterized by short cycles with heavy periods; however, some women who are anovulatory have long cycles and light, infrequent periods.
Ovulatory menstrual cycles tend to be regular and predictable in terms of duration and heaviness of bleeding.
Having short menstrual cycles (less than 21 days), or long menstrual cycles (longer than 36 days) can be a sign that you are anovulatory
Abnormal uterine bleeding due to ovulatory dysfunction (AUB-O) is an irregular anovulatory uterine bleeding that, after pelvic examination and pelvic ultrasound, cannot be attributed to structural abnormalities in the uterus, such as endometrial inflammation, cancer, complications of pregnancy, use of oral contraceptives, IUDs, systemic disorders, or certain drugs.
Anovulatory bleeding is common at the beginning and end of reproductive age.
Anovulatory bleeding occurs in the absence of bleeding disorders (coagulopathies) or platelet dysfunction because coagulopathies can cause abnormal bleeding
Chronic anovulation can lead to long term problems, such as obesity, hirsutism, central adiposity, infertility, hyperandrogenism or osteopenia. Women with chronic anovulation are at higher risk of developing stress fractures, especially in the lower extremities
Causes
What causes chronic anovulation?
- Pathological causes of Anovulation
Hyperandrogenic chronic anovulation is very common in women with polycystic ovary syndrome (PCOS). Other pathological causes of chronic anuvolation include follicle atresia, abnormal gonadotropin secretion, hypothalamic, pituitary and endocrine dysfunction, inappropriate hormonal feedback (in liver disease), functional androgen excess (ovarian or adrenal).
- Psychogenic Factors in Anovulatory Women (stress-induced anovulation)
Common psychogenic causes of anovulation include stress and emotional lability
- Association between anovulation and lifestyle cultural customs (Diet and Lifestyle)
Common causes for anovulatory cycles are physical overexertion, and eating habits (food, eating behavior, dietary habits, food traditions, diets). When women are overweight, their bodies will react differently to hormonal fluctuations as they occur. Obesity contributes to excessive extraglandular production of estrogen
Treatment
How to treat anovulation?
- Classical treatment
A cyclic hormone replacement therapy is recommended to induce ovulation, Clomiphene citrate (Clomid) is a nonsteroidal medication used to induce ovulation, especially in women with polycystic ovary syndrome or hypothalamic secondary amenorrhea. Treatment starts with a low initial dose, 50 mg per day orally for 5 days per cycle, usually from cycle day 3 to cycle day 7. The dose may be increased to 100 mg per day orally for 5 days per cycle. If ovulation occurs and pregnancy is not achieved, treatment should be continued in the two next cycles with 100 mg per day orally for 5 days per cycle, from day 3 to day 7 day of the cycle.
Cyproterone acetate (CPA, Androcur, Cerpafar) is an antiandrogen and progestogen used in the treatment of hirsutism. Treatment is started with a lower dose of 100 mg daily in divided doses (1 tablet 50 mg twice daily). The maximum daily dose is 300mg.
Spironolactone (Aldactone) is a diuretic or water pill used in the treatment of female hirsutism. Treatment is started with a lower dose of 100-200 mg/day orally for 6 months. Spironolactone has antiandrogenic effects that may enhance treatment of severe hirsutism. The effect of a combination therapy with an oral contraceptive or with dexamethasone is completely beneficial
Next steps management
How to diagnose anovulation?
Functional diagnostic tests are used to establish the ovulatory and anovulatory menstrual cycles. These tests can include CBC, FSH, TSH, LH, serum DHEAS, prolactine, etc.
CT or MRI of the sella to check for pituitary neoplasm, surgical treatment indicated once neoplasm is confirmed
Ovarian imaging tests, such as pelvic ultrasonography (US) are commonly used in the diagnosis of PCOS, especially in patients who are being evaluated for ovulatory dysfunction or hyperandrogenism
For patients with polycystic ovary syndrome who are actively trying to conceive: clomiphene citrate 50-100mg/day for 5 days to induce ovulation; Administration of clomiphene citrate in combination with 450 IU of gonadotropins (Menopur 75IU or Gonal-f®). Ovarian stimulation will be initiated with a combination of highly purified urinary FSH and LH, such as Menopur 75IU (each vial contains 75 IU FSH activity and 75 IU LH activity) or with a combination of recombinant FSH and Rec LH, such as Gonal-f® (follitropin alfa for injection). Administration of clomiphene citrate in combination with 225 IU of gonadotropins (Rec FSH, Gonal-f®) and GnRH antagonists (GnRH-a, Degarelix). Women should receive 20 mg of Degarelix on the 1st day of menstruation followed by a standard dose of 225 IU of Rec FSH on the second day until the day of ovulation triggering.
For women with PCOS who want to avoid pregnancy: medroxyprogesterone acetate 5-10 mg/day for two weeks every one or two months
Oral contraceptives are recommended to reduce the risk of endometrial hyperplasia and cancer
References
Verified by: Dr.Diab (December 3, 2017)
Citation: Dr.Diab. (December 3, 2017). What is Chronic Anovulation? Causes Symptoms and Treatment. Medcoi Journal of Medicine, 12(2). urn:medcoi:article15546.












There are no comments yet
Or use one of these social networks