Myocardial Infarction volume and management using Cardiac Biomarkers
[pro_ad_display_adzone id=”17752″]
Coronary artery disease or ischemic heart disease is a group of cardiovascular diseases that includes: stable and unstable angina, myocardial infarction (MI), and sudden cardiac death. CAD was the most common cause of death globally. [1]
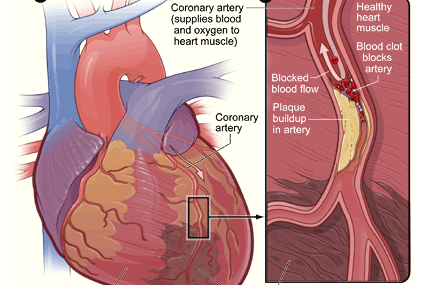
Myocardial Infarction or myocardial ischemias are mainly caused by atherosclerotic arterial stenosis resulting from fats building up in the arteries. Atherosclerosis is a gradual process, which increases overtime. The main symptom of MI is chest pain persisting for more than 30 min accompanied with a migrating discomfort which may travel into the left shoulder, arm, neck, back (interscapular), or the lower jaw. Occasionally it may feel like a stabbing knife or a persisting heartburn that is not released by taking a nitroglycerin pill. Other symptoms include shortness of breath and sometimes symptoms are absent. Less commonly complications such as heart failure or an irregular heartbeat (arrhythmia) may present.
Major risk factors for CAD include systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg, total cholesterol ≥240 mg/dL, cigarette smoking, diabetes mellitus.
In incident cases of non fatal myocardial infarction (MI) and CHD death was investigated. Eighty-seven percent to 92% of cohort participants with fatal CHD had at least one antecedent major RF. Likewise, 92% of men and 87% of women with nonfatal MI had exposure to at least one major RF.[2]
Diagnosis
A number of tests are available for the diagnosis of MI, such tests include: electrocardiogram, cardiac stress testing, coronary computed tomographic angiography, CT, and coronary angiogram, among others
Disease and drug-related biomarkers
Disease related biomarkers give an indication of underlying pathological processes such as an already existing disease (diagnostic biomarker), or show the therapeutic prognosis in a patient (the probable effect of a treatment in a patient, predictive or risk indicator), or may show the outcome of a disease in a patient and how the pathological and functional disorder may develop in a patient regardless of the therapeutic intervention (pathological outcome regardless of the treatment course, prognostic biomarker).
Cardiac biomarkers are used in the diagnosis procedure and risk stratification of patients with suspected acute coronary syndrome and those presenting with chest pain. The cardiac troponins are the cardiac markers of choice for patients with acute coronary syndrome..
| Current Cardiac Biomarkers | Cardiac Biomarkers of minor importance |
|
|
| Table : Current “Major” and past “Minor” Cardiac Biomarkers | |
CK-MB has high specificity for cardiac tissue, an elevated CK-MB is relatively specific for cardiac muscle injury, especially in patients presenting with ischemic symptoms when skeletal muscle damage is not present. Assays for CK-MB can be performed easily and rapidly.
The relative index calculated by the ratio of CK-MB (mass) to total CK can assist in differentiating false-positive elevations of CK-MB arising from skeletal muscle.
A ratio < 3 is consistent with a skeletal muscle source, while ratios > 5 are indicative of a cardiac injury. Ratios between 3 and 5 require further evaluation.
Creatinine Kinase starts rising in the blood 4-6 hours after the onset of chest pain. It peaks at 10-24 hours and then returns to normal after 48-72 hours. Since CK levels return to baseline 48 to 72 hours after infarction, it can be used to detect reinfarction.
New elevations that occur after normalization are indicative of recurrent injury, again with the caveats in regard to sensitivity and specificity indicated above. However, for these reasons, CK-MB cannot be used for late diagnosis
Cardiac Troponins (cTn) are the preferred biomarker for the diagnosis of acute MI because they are more specific compared to CKMB in detection of infarction, cTn control the calcium-mediated interaction of actin and myosin. It exists in three isoforms: troponin C, troponin I and troponin T. whereas Troponin I is completely specific for the heart.
Cardiac troponins begin rising in the blood 4-6 hours post infarction (same time as CKMB).
It peaks in 12-24 hours but may take weeks to return to normal
Myoglobin is a heme protein found in skeletal and cardiac muscle, myoglobin typically rises 2-4 hours after onset of infarction, peaks at 6-12 hours, and returns to normal within 24-36 hours. Rapid myoglobin assays are available, but overall, they have a lack of cardio specificity.
Serial sampling every 1-2 hours can increase the sensitivity and specificity of myoglobin:
A rise of 25-40% over 1-2 hours is strongly suggestive of acute MI. However, in most studies, so the negative predictive value of myoglobin for acute MI is high enough ~10% to exclude the diagnosis of acute MI, as myoglobin only achieved 90% sensitivity for acute MI.[3]
Quantitative Imaging Biomarkers
CT (Computerized Tomography), MRI (Magnetic Resonance Imaging), and PET (Positron Emission Tomography) support functional imaging, which help exploring atherosclerotic plaques, calcifications and other structural abnormalities relevant to vascular permeability and blood flow.
F-MRI and F-PET supports dynamic imaging, which provide a much deeper molecular dimension while monitoring time relevant changes, ex. Heart beating, receptor blockage, etc…
Promising imaging biomarkers for cardiovascular diseases identified at IBS II.
- Dynamic contrast enhanced-MRI (DCE-MRI): measures blood flow/vascular permeability [6]
Prevention can be made by
- Lifestyle modifications (eating a healthy diet, regular exercise, maintaining a healthy weight, abiding from bad lifestyle habits i.e. not drinking and not smoking).
- Medications, taking medicaments for specific underlying diseases such as taking drugs to treat diabetes, high cholesterol level, or high blood pressure.
- Regular screening for people who are at low risk and do not have symptoms
References
Verified by: Dr.Diab (November 14, 2017)
Citation: Dr.Diab. (November 14, 2017). Myocardial Infarction volume and management using Cardiac Biomarkers. Medcoi Journal of Medicine, 9(2). urn:medcoi:article16309.












One comment
Or use one of these social networks